Medicare Supplements: Filling Those Gaps
So what do you do about the out-of-pocket exposure Original Medicare leaves you with?
One option is to keep Original Medicare and add a Medicare Supplement policy with a stand-alone drug plan. Also known as Medigap policies, Medicare Supplements feature monthly premiums, but they work with all health care professionals. They can also save you money if you’re hospitalized and need health services for extended periods of time.
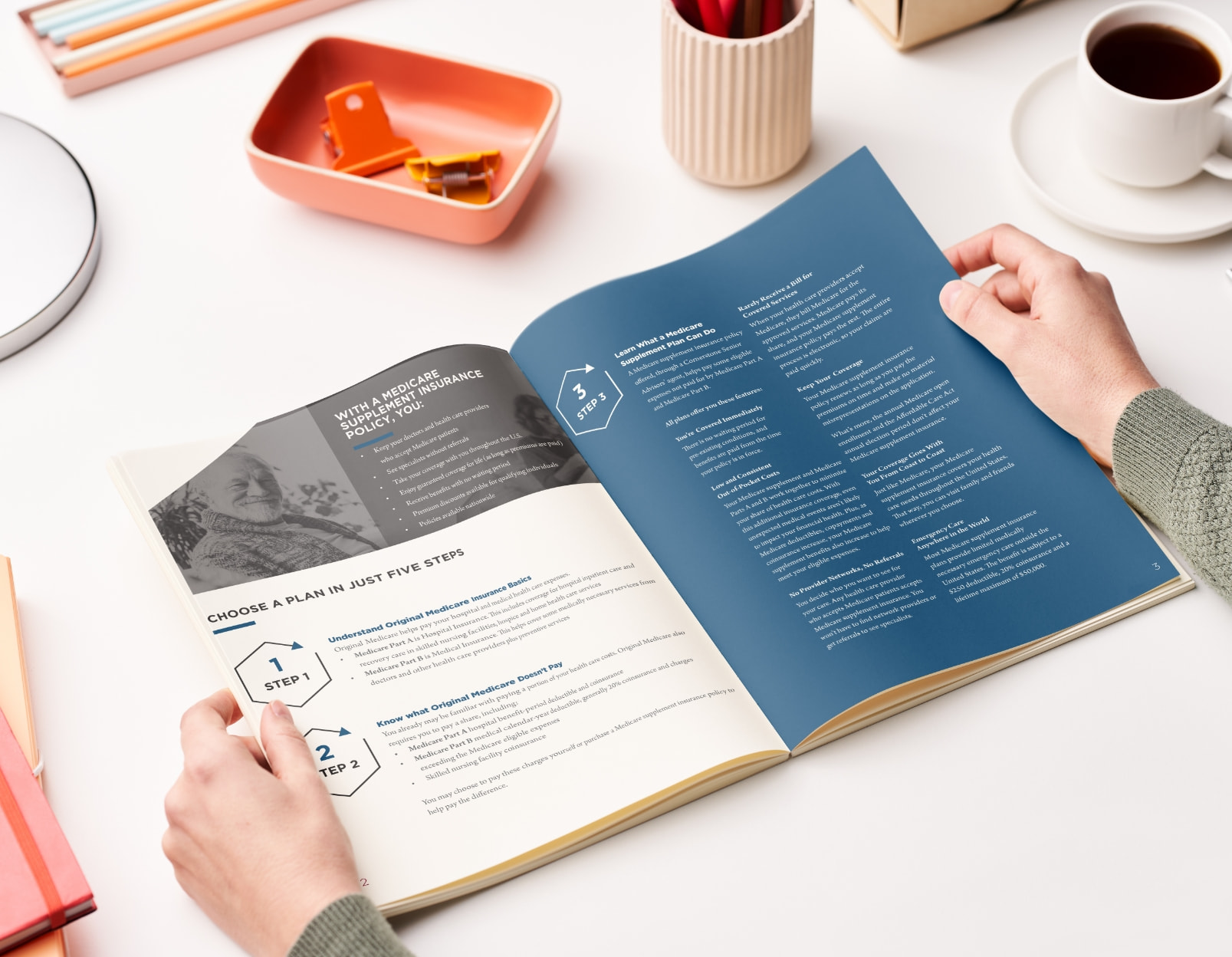
Choose a Supplement in Five Easy Steps
This easy-to-follow, 8-page guide will walk you through five keys to choosing a Medicare Supplement insurance policy that’s right for you. In this guide, you’ll learn:
Benefits and key features of Medicare Supplement plans
Budgeting costs to consider
Summaries of select Supplement plans
A glossary of important terms

Popular Medicare Supplement Plans Medicare Supplement Plan F
As far as coverage goes, Plan F is very simple to explain. It fills all the gaps!
When you combine a Plan F with Medicare, you have no network and no out-of-pocket exposure. All you will receive in the mail is a statement of benefits paid.
But here’s the catch: Plan F was so popular that the government discontinued it, making it no longer available to new Medicare beneficiaries after January 2020. Only those grandfathered into the plan can continue using Supplement Plan F.
Medicare Supplement Plan G
Plan G is currently the most popular Medicare Supplement plan. It is just like Plan F with one difference: it does not cover your Part B deductible of $240 (remember, this is an annual deductible).
As far as Part A of Medicare, your hospitalization, plan G picks up where Medicare leaves off and pays 100% of the balance. In other words, when you combine a Plan G with Medicare, you can use any health care professional that accepts Medicare and you have a one-time annual deductible of $240. Once this deductible has been paid, the plan kicks in and all remaining costs are covered.


Medicare Supplement Plan N
Plan N is just like G and F as far as hospitalization goes: It will pick up 100% of the costs you are left with after Medicare pays. The difference with Plan N falls outside of the hospital.
With Plan N, you will have to pay your Part B annual deductible of $240, just like with plan G. Once this deductible has been met, you will have copays of $20 or less when you see a primary care doctor or specialist and $50 for emergency room visits.
The aspect of Plan N that tends to intimidate people is it doesn’t cover the Part B excess charge. Medicare allows doctors to charge up to 15% more than what Medicare assigns. If you ever go to a health care professional who chooses to take advantage of that 15% excess charge, you are required to pay it under Plan N. (Plans F and G are the only plans that pay the 15% excess charge.)
LET'S TALK You’re Not Alone
Choosing the right Medicare Supplement or Medicare Advantage plan can seem daunting, but it doesn't need to be. We're here to make this journey easier.